The TLT Treatment Breakthrough
Although TLT sounds complicated, it uses our existing FDA-cleared, high-power, near-infrared lasers in a new manner. It's a fast, non-drug treatment for PTSD and non-acute TBI. A new and promising research study involving the Manhattan Beach Protocol for TLT treatment of PTSD and TBI is now available. For more information about the Manhattan Beach protocol of high-dose transcranial laser therapy in PTSD, TBI, and CTE, please go to the inquiry form.
TLT has the potential to speed up PTSD treatment by 10X, reduce cost by 4X, and vastly improve outcomes. A standard regimen of TLT has been shown to reduce sleep disturbances and suicidal thoughts in 100% of a small series of patients. TLT also reduced depression, as measured by the BDI, by about 50%. TLT did all of this in just 10 treatments. You can receive one treatment as often as daily. Read more about this new PTSD treatment in the news
95% Reduction in Symptoms
Using our advanced treatment protocol, we have achieved a 95% reduction in the symptoms of PTSD and TBI. Here is a graph of a patient's scores on a measure of PTSD and depression. It shows that even 4 months after treatment, the improvement "sticks."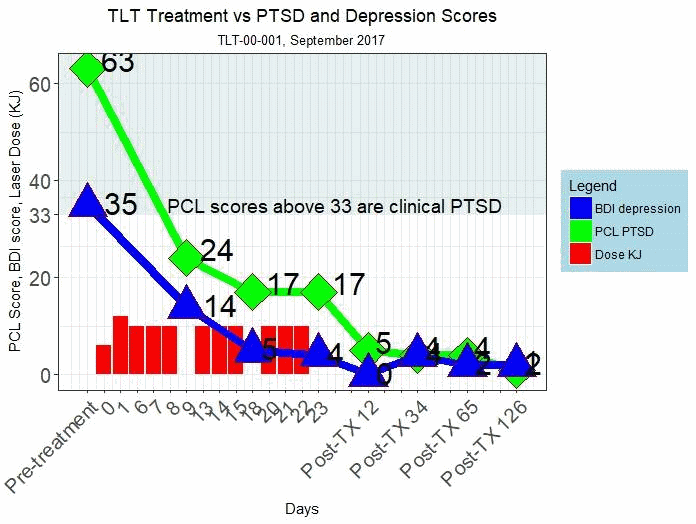
More about PTSD
1 in 5 vets from our Iraq and Afghanistan wars have PTSD. Sadly, veterans account for 1 in 5 suicides. More than $2B has been spent on veterans' PTSD. Often, it helps, but results are sporadic and often incomplete. Most of the time, though, the 700,000+ vets with PTSD will not receive treatment. Current treatments are estimated to cost $5000 or more PER YEAR.With current treatments, we would have to spend $70 Billion to give all the vets with PTSD treatment for the next twenty years. And not all of them would benefit.
TLT Treatment for PTSD & Chronic TBI
The devastating impact of untreated or undertreated PTSD does not stop with the patient. Their families suffer as well, and so does society, partly because of the very high unemployment rate among those with PTSD.TLT has the potential to make a dramatic difference in the battle against PTSD. It takes just 1-3 weeks of therapy, versus 10-20 weeks for standard regimens. Initial results from TLT show improvement that exceeds virtually all other treatment regimens.
TLT Treatment for PTSD & TBI
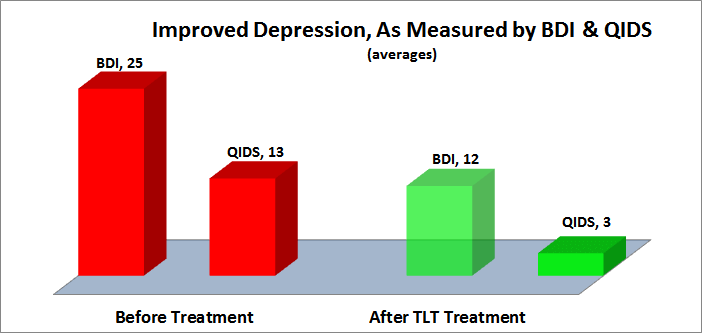
In 2015, a Denver group reported their results from a series of ten patients with PTSD & TBI treated with TLT. Using TLT with the "Denver protocol," the results are very impressive.DEPRESSION
Depression was assessed using both the Quick Inventory of Depressive Symptomatology, QIDS, and the Beck Depression Inventory, BDI.The QIDS decreased 75% from 13, moderately depressed, to 3, normal. The BDI-II decreased 50% from an average of 25, moderately depressed, to an average of 12, minimal depression. The following chart illustrates the substantive decreased in depression following TLT.
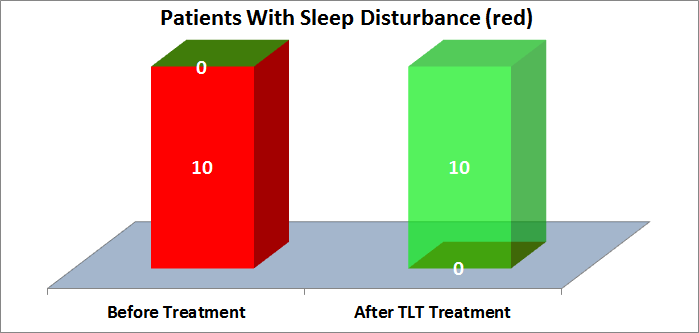
SLEEP DISTURBANCE
Sleep disturbances, nightmares, and insomnia are PTSD hallmarks. They are also the least likely PTSD symptoms to be treated successfully with current approaches.Sleep is the body's natural PTSD salve, helping with the consolidation of fear extinction memory. Nightmares and insomnia interfere with this process. A vicious cycle can occur, with sleep disturbances exacerbating PTSD, which in turn exacerbates sleep disturbances.
TLT may represent a breakthrough in treatment of PTSD sleep disturbances. As shown in the graph below, 10 of 10 patients with sleep disturbances reported substantial or total improvements after TLT.
ANXIETY
Anxiety is one of the hallmarks of PTSD. Current PTSD therapies can treat anxiety, and the Denver report indicates that TLT may be one of the best modalities. As shown in the graph below, 9 of 9 patients with anxiety were successfully treated with TLT.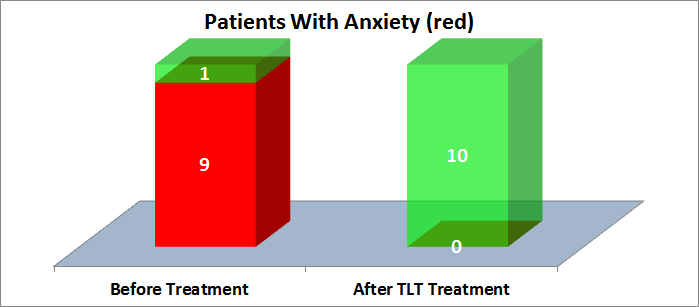
SUICIDE
Statistics from the VA indicate that suicide rates are two times higher for vets than for civilians. Most studies indicate that PTSD puts vets at further risk of suicide. In the Denver report, 5 of 10 patients had suicidal thoughts, and all 5 were successfully treated with TLT, as shown in the chart below.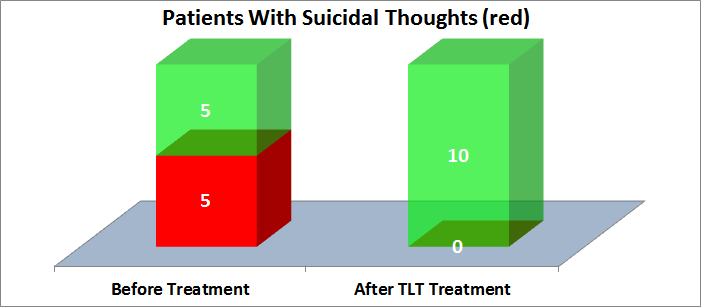
UNEMPLOYMENT
Unemployment is more closely correlated with PTSD severity than depression. Unemployment can be both a cause of worse PTSD symptoms, and the result of PTSD symptoms. In either case, PTSD-related unemployment takes its toll on PTSD patients, families, and society. Impressively, of the 6 patients who were unemployed, 5 of them found gainful employment after TLT, as shown in the following chart.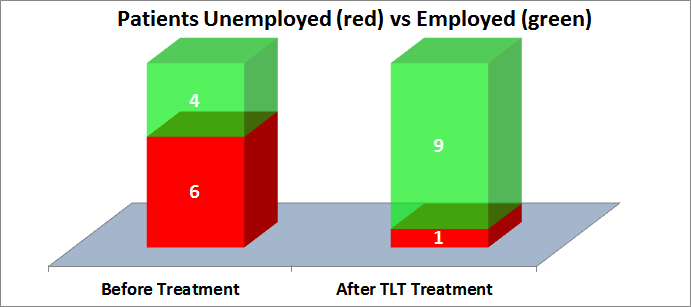
SUBSTANCE ABUSE
Substance abuse is a common comorbidity with PTSD. It can exacerbate, and also result from, PTSD. Two of 10 patients reported substance abuse pre-treatment, and after TLT treatment none reported substance abuse, as shown in the following chart: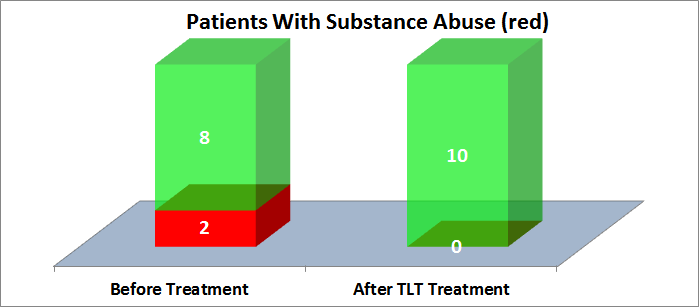
TLT Treatments for PTSD & TBI
TLT is a pain-free, drug-free, needle-free, effort-free treatment. No special preparation before or after each TLT session is needed. Patients remain clothed, put on special goggles to protect their eyes from the high intensity near-infrared laser, and sit or lay down. The laser therapist then applies the laser light to selected head regions for 10-30 minutes. Most patients report a soothing warm feeling during the treatment. Simulated TLT is demonstrated in the photo below:
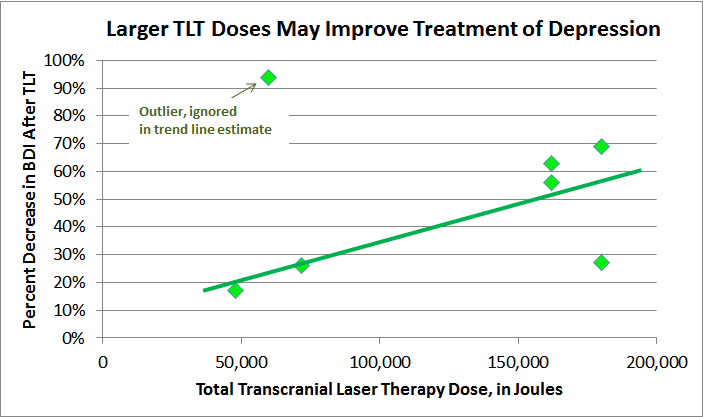
There are two protocols in use, the Denver and the Manhattan Beach protocols. Each patient's therapy is individually determined, and is based on either the Denver or Manhattan Beach protocol. These protocols serve as the standard, but each individual treatment plan may vary. The Manhattan Beach protocol uses higher laser power, more total Joules of laser, and more rapid treatments. The results from treatment with the Denver protocol suggests that higher total Joules results in more improvement in depression. However, the sample size is too small to be statistically significant. As the following chart shows, the relationship between total Joules and depression improvement needs further investigation to determine the dose-response curve.
DENVER PROTOCOL
The standard Denver protocol is 2,400 - 3,000 Joules per treatment per location. In each session, 2-3 locations are treated. Both temporal/cortical areas "A" are always treated, and in some patients area "B" is also treated. There are either 10 or 20 sessions, one per week, for 10-20 weeks. Total Joules are 50,000 - 180,000. The therapy is a 10 Watt, 10 Hz pulsed beam from an 810/980 nM LiteCure laser.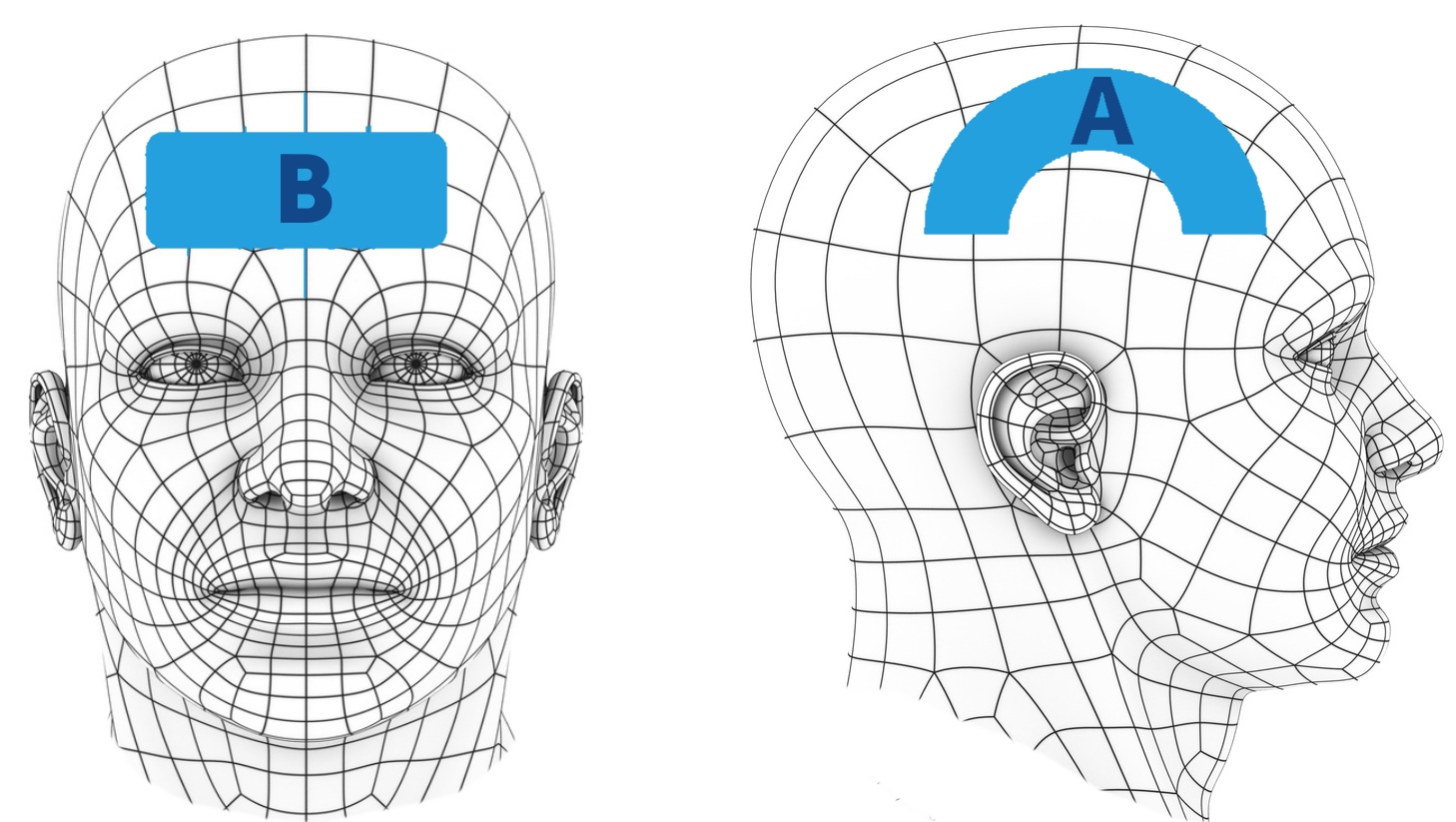
MANHATTAN BEACH PROTOCOLS
The Manhattan Beach protocol is 3,000 - 7,500 Joules per treatment per location. In each session, 3 locations are treated. Both temporal/cortical areas "A" and area "B" are treated, but both areas are expanded somewhat compared with the Denver protocol. There are 2-5 sessions per week over 2-4 weeks. Total Joules are 80,000 - 300,000. The therapy is a 15-25 Watt, continuous or 10 Hz pulsed beam from an 810/980 nM LiteCure laser.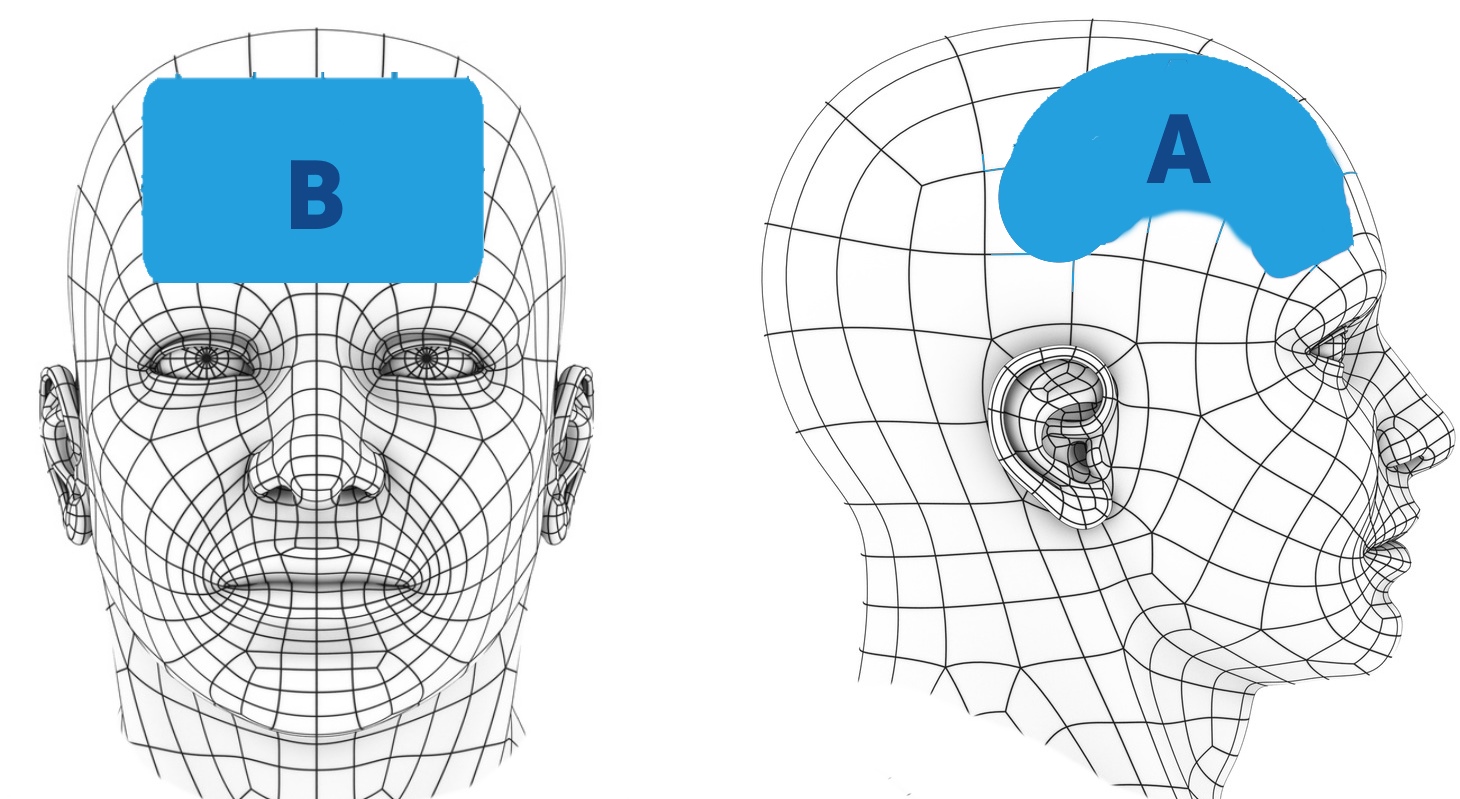
Relationship Between PTSD & TBI
There is substantial overlap between PTSD & TBI, in terms of symptoms, treatment, comorbidity, and treatment. The same event that caused TBI can also cause PTSD, such as accidents or combat.Headache is the most common symptom of chronic TBI, and is a common symptom in PTSD. Suicide is more common among both chronic repetitive TBI and PTSD patients. Both TBI & PTSD have numerous co-morbid associated conditions. Anxiety is a hallmark of PTSD, and is very common in TBI. Head, neck and back pain is commonly seen, ~ 20-50%, in both conditions. Depression is common in both groups.
Both TBI & PTSD have shown positive results from cognitive therapy and near-infrared light. Although a single recent study claims to be able to distinguish PTSD from TBI using SPECT, the utility of this differentiation is uncertain given that the treatments are often the same, the treatments for both are imperfect, and the conditions are often co-morbid.
Science of TLT Treatments for PTSD & TBI
The most important report to date for using TLT to treat PTSD and TBI is "Treatments for traumatic brain injury with emphasis on transcranial near-infrared laser phototherapy", the sentinel article by Morries, Cassano, and Henderson. They treated 10 patients with TBI/PTSD with high-power 10 W laser 810/980 nm, with outstanding results, as illustrated in the graphs in other sections. To understand the scientific underpinnings of why this therapy should work, requires examining five overlapping areas: (1) The neuroanatomy and neurocircuitry of PTSD and TBI, (2) the overlap of PTSD and TBI, (3) numerous animal studies showing the benefits of laser light in animal models of TBI, (4) basic neuroanatomy as it relates to (1) and to the A-B areas in the Denver and Manhattan Beach protocols, and (5) what kinds of lasers are able to penetrate the human skull into the cortex.Many studies have examined the brain structures involved in PTSD. Consistent findings include
- hyperactive bilateral amygdala, with smaller left amygdala volumes
- hyperactive mid and dorsal anterior cingulate cortex, with smaller volumes
- hypoactive ventromedial prefontal cortex, which is associated with increased amygdala activity
- hypoactive inferior frontal gyrus
- smaller hippocampal volumes
- hypoactive Broca's area
In stroke, near infrared laser also shows promise: Low-level laser therapy applied transcranially to rats after induction of stroke significantly reduces long-term neurological deficits. Apoptosis, or programmed cell death, resulting from cerebral ischemia, may be reduced by LLLT in rats.
Studies in mice showed that the the 808nm wavelength light penetrated skull and brain much better than the 660 or 940nm wavelengths.
Two recent studies show that only high-power near infrared lasers of at least 10 W are capable of penetrating sheep or human skulls and reaching the brain with the kinds of energy required to replicate animal studies. Low level light therapy, cold lasers, were similarly shown to be unable to penetrate the skull. Although many rat and mouse studies show an effect of LLLT, this is consistent with the non-transmission of LLLT through human skulls because LLLT is a mouse-sized laser, and the equivalent human-sized laser is high-power, 10 W or more. It is completely expected that a mouse-sized dose of laser light will not work in humans.
Other Treatments for PTSD
Cognitive therapy
The most standard treatment, cognitive or psychotherapy, has good but variable results. According to a review of 36 trials published in JAMA in the summer of 2015, trials of psychotherapy "... have shown clinically meaningful improvements for many patients with PTSD. However, nonresponse rates have been high, many patients continue to have symptoms, and trauma-focused interventions show marginally superior results ... There is a need for improvement in existing PTSD treatments..." To treat the persistent PTSD, there is a need to focus on following three areas:- Assessment of appropriate problem that need to be focused to modify the threat of trauma
- There is a need to expand the trauma memory in the context of personal experiences to decrease the disturbance.
- Removal of the cognitive strategies and dysfunctional behavior causes that prevent the elaboration of traumatic memory and aggravate symptoms.
One of the effective options in cognitive therapy is thought suppression experiments. The thoughts of trauma increase the chances of stress, so suppression of thoughts (Ehlers & Clark, 2000). An imagery rescripting technique used for patients who fight with upsetting, disturbing imagery. Imaginal exposure combined with rescripting promotes the conceptual processing, which is beneficial in PTSD treatment (Kar, 2011). All types of techniques used in cognitive-behavioral therapy altered the regulation of fear and emotional distress by altering the neural circuits and effect the left orbitofrontal cortex (Porto et al., 2009).
Eye Movement Desensitization and Reprocessing Therapy
Eye movement desensitization and reprocessing therapy are highly effective psychotherapy therapy for PTSD. It is as effective as cognitive therapy, but how it affects the nervous system to diminish the stress still not clear, but possible Treatment Mechanisms in Eye movement desensitization and reprocessing described in Table 1 (Gunter & Bodner, 2009).Disturbance in working memory: Disruption of the traumatic recollection in working memory
Increased hemispheric communication: Neurological communication across the two brain hemispheres
Psychological distancing/ detached processing: Evocation of a sense of psychological distance from trauma
Reciprocal inhibition: Coupling of traumatic recollection and Relaxation
Orienting response: Relaxation and/or cognitive flexibility
REM: Evocation of an REM-like mind-brain state
Disturbance in working memory acts as a distractor task that actually interfere in traumatic memories. Rapid eye movement produced greater benefits in eye movement desensitization and reprocessing therapy than slow movement because rapid eye movement allows better distraction than a slow one (Gunter & Bodner, 2009). According to Alan Baddeley (2000), central executive performs the cognitive functions of higher order. Multitasking and distraction during eye movement therapy cause disturbance in the central executive system to provide the benefits in PTSD.
According to Propper and Christman (2008) proposed that increased hemispheric communication that involved the neurological communication across the two brain hemispheres is the underlying mechanism in eye movement desensitization and reprocessing therapy. In their account, horizontal eye movements can enhance the retrieval of episodic trauma memories for further reprocessing to decrease the traumatic distress. According to Gunter and Bodner research eye movements increased the functioning of parasympathetic nervous system as compared to sympathetic system that decreases the stress by dearousal (Gunter & Bodner, 2009).
Drug Therapy
Drug therapy, along with cognitive therapy, are standard PTSD treatmetns. Practice guidelines recommend the selective noradrenaline reuptake inhibitors (SNRIs) and selective serotonin reuptake inhibitors (SSRIs). The pathophysiology of PTSD relates in part to sympathetic and serotonergic systems. The serotonergic system is involved in behavioral regulation, emotional processing and cognition, so stimulation of this system cause the disturbance in normal regulations (Bailey, Cordell, Sobin, & Neumeister, 2013). The serotonergic signaling in the amygdala regulates fear and threat responsiveness. Venlafaxine is the most commonly used drugs in PTSD because it blocks the reuptake of both 5-HT and NE to decrease the signaling in the amygdala. 5-HT1A receptor agonist (Buspirone) and 5-HT2A receptor antagonist (Nefazodone) also provide beneficial effects in PTSD (Bailey et al., 2013; Cain, Maynard, & Kehne, 2012).The adrenergic receptors enhance the sympathetic responses and central nervous system activity through cell bodies located in the locus coeruleus and projects to the prefrontal cortex and limbic system structures (like hypothalamus and amygdala) (Bailey et al., 2013). The hyperarousal in PTSD related with sleep disturbance and nightmare and these symptoms are not treated with SSRI. Use of a1-adrenergic receptor antagonist, prazosin decreased these symptoms in PTSD. Propranolol which block the Beta receptors also decrease the stimulatory effect of the sympathetic system in PTSD (Cain et al., 2012).
Drugs like benzodiazepines, which are GABA receptor agonist decrease the stimulation due to its inhibitory nature. Use of diazepam in acute PTSD decrease the symptoms in a few hours of administration. It prevents the fear, sleep disturbance and nightmares to a significant extent. Other drugs that provide the benefits in PTSD are a-2 agonists, monoamine oxidase inhibitors, opioid antagonists, NMDA antagonists, and lithium carbonate (Kapfhammer, 2014).
Read More About PTSD & TLT
Depressing PTSD FactsSpecific PTSD & TLT References
- A. Baddeley, "The episodic buffer: A new component of working memory?," Trends in Cognitive Sciences, vol. 4, no. 11, pp. 417-423, 2000 [Online]. Available: View
- A. Ehlers and D. M. Clark, "A cognitive model of posttraumatic stress disorder," Behaviour Research and Therapy, vol. 38, pp. 319-345, 2000 [Online]. Available: View
- A. Etkin and T. D. Wager, "Functional Neuroimaging of Anxiety: A Meta-Analysis of Emotional Processing in PTSD, Social Anxiety Disorder, and Specific Phobia," AJP, vol. 164, no. 10, pp. 1476-1488, Oct. 2007 [Online]. Available: View
- A. Karl, M. Schaefer, L. S. Malta, D. Dörfel, N. Rohleder, and A. Werner, "A meta-analysis of structural brain abnormalities in PTSD," Neuroscience & Biobehavioral Reviews, vol. 30, no. 7, pp. 1004-1031, 2006 [Online]. Available: View
- Available: View
- B. Kovachy, R. O'Hara, N. Hawkins, A. Gershon, M. M. Primeau, J. Madej, and V. Carrion, "Sleep Disturbance in Pediatric PTSD: Current Findings and Future Directions," J Clin Sleep Med, vol. 9, no. 5, pp. 501-510, May 2013 [Online]. Available: View
- B. Theeler, S. Lucas, R. G. Riechers, and R. L. Ruff, "Post-traumatic headaches in civilians and military personnel: a comparative, clinical review," Headache, vol. 53, no. 6, pp. 881-900, Jun. 2013.
- C. A. Raji, K. Willeumier, D. Taylor, R. Tarzwell, A. Newberg, T. A. Henderson, and D. G. Amen, "Functional neuroimaging with default mode network regions distinguishes PTSD from TBI in a military veteran population," Brain Imaging and Behavior, vol. 9, no. 3, pp. 527-534, Sep. 2015 [Online]. Available: View
- C. E. Tedford, S. DeLapp, S. Jacques, and J. Anders, "Quantitative analysis of transcranial and intraparenchymal light penetration in human cadaver brain tissue," Lasers Surg. Med., vol. 47, no. 4, pp. 312-322, Apr. 2015 [Online]. Available: View
- C. J. Bryan and T. A. Clemans, "Repetitive traumatic brain injury, psychological symptoms, and suicide risk in a clinical sample of deployed military personnel," JAMA Psychiatry, vol. 70, no. 7, pp. 686-691, Jul. 2013.
- C. K. Cain, G. D. Maynard, and J. H. Kehne, "Targeting memory processes with drugs to prevent or cure PTSD," Expert Opin Investig Drugs, vol. 21, no. 9, pp. 1323-1350, 2012 [Online]. Available: View
- C. Kunsman, "Under Much Grace: Post Traumatic Stress as a Physical Process and the Inadequacies of Some Types of Biblical Counseling: Understanding Doctrine Over Person, Part VIII," Under Much Grace. 12-Jan-2012 [Online]. Available: View
- C. R. Bailey, E. Cordell, S. M. Sobin, and A. Neumeister, "Recent Progress in Understanding the Pathophysiology of PostTraumatic Stress Disorder: Implications for Targeted Pharmacological Treatment," CNS Drugs, vol. 27, no. 3, pp. 221-232, 2013 [Online]. Available: View
- D. Dobbs, "The PTSD Trap: Our Overdiagnosis of PTSD In Vets Is Enough to Make You Sick," WIRED, 22-Mar-2012. [Online]. Available: View
- D. X. Cifu, B. C. Taylor, W. F. Carne, D. Bidelspach, N. A. Sayer, J. Scholten, and E. H. Campbell, "Traumatic brain injury, posttraumatic stress disorder, and pain diagnoses in OIF/OEF/OND Veterans," J Rehabil Res Dev, vol. 50, no. 9, pp. 1169-1176, 2013.
- E. A. Walker, E. Newman, D. J. Dobie, P. Ciechanowski, and W. Katon, "Validation of the PTSD checklist in an HMO sample of women," General Hospital Psychiatry, vol. 24, no. 6, pp. 375-380, Nov. 2002 [Online]. Available: View
- E. B. Foa, T. M. Keane, M. J. Friedman, and J. A. Cohen, Effective Treatments for PTSD: Practice Guidelines from the International. New York: The Guilford, 2009 [Online]. Available: View
- E. Blanchard, "Psychometric properties of the PTSD checklist (PCL)," Behaviour Research and Therapy, vol. 34, no. 8, pp. 669-673, Aug. 1996 [Online]. Available: View
- E. Vermetten and J. D. Bremner, "Circuits and systems in stress. II. Applications to neurobiology and treatment in posttraumatic stress disorder," Depress. Anxiety, vol. 16, no. 1, pp. 14-38, Jan. 2002 [Online]. Available: View
- G. Sartory, J. Cwik, H. Knuppertz, B. Schürholt, M. Lebens, R. J. Seitz, and R. Schulze, "In Search of the Trauma Memory: A Meta-Analysis of Functional Neuroimaging Studies of Symptom Provocation in Posttraumatic Stress Disorder (PTSD)," PLoS ONE, vol. 8, no. 3, p. e58150, Mar. 2013 [Online]. Available: View
- H. Bono, S. Kawano, H. Ono, and T. Takagi, "Tutorial videos of bioinformatics resources: Online distribution trial in Japan named TogoTV," Briefings in bioinformatics, vol. 13, no. 2, pp. 258-68, 2012.
- H. Cohen and P. D. ~ 3 min read, "An Overview of Post-Traumatic Stress Disorder (PTSD)," Psych Central.com. [Online]. Available: View
- H.-P. Kapfhammer, "Patient-reported outcomes in post-traumatic stress disorder. Part II: Focus on pharmacological treatment," Dialogues in Clinical Neuroscience, vol. 16, no. 2, pp. 227-237, 2014 [Online]. Available: View
- J. D. Bremner, M. Narayan, E. R. Anderson, L. H. Staib, H. L. Miller, and D. S. Charney, "Hippocampal Volume Reduction in Major Depression," AJP, vol. 157, no. 1, pp. 115-118, Jan. 2000 [Online]. Available: View
- J. E. Sherin and C. B. Nemeroff, "Post-traumatic stress disorder: the neurobiological impact of psychological trauma," Dialogues Clin Neurosci, vol. 13, no. 3, pp. 263-278, Sep. 2011 [Online]. Available: View
- J. H. Krystal, T. R. Kosten, S. Southwick, J. W. Mason, B. D. Perry, and E. L. Giller, "Neurobiological aspects of PTSD: Review of clinical and preclinical studies," Behavior Therapy, vol. 20, no. 2, pp. 177-198, Mar. 1989 [Online]. Available: View
- J. Khuman, J. Zhang, J. Park, J. D. Carroll, C. Donahue, and M. J. Whalen, "Low-level laser light therapy improves cognitive deficits and inhibits microglial activation after controlled cortical impact in mice," J. Neurotrauma, vol. 29, no. 2, pp. 408-417, Jan. 2012.
- J. L. Gradus, M. K. Suvak, B. E. Wisco, B. P. Marx, and P. A. Resick, "TREATMENT OF POSTTRAUMATIC STRESS DISORDER REDUCES SUICIDAL IDEATION: Research Article: PTSD Treatment Reduces Suicidal Ideation," Depression and Anxiety, p. n/a-n/a, Apr. 2013 [Online]. Available: View
- K. Krysinska and D. Lester, "Post-traumatic stress disorder and suicide risk: a systematic review," Arch Suicide Res, vol. 14, no. 1, pp. 1-23, 2010.
- K. Matsuo, K. Taneichi, A. Matsumoto, T. Ohtani, H. Yamasue, Y. Sakano, T. Sasaki, M. Sadamatsu, K. Kasai, A. Iwanami, N. Asukai, N. Kato, and T. Kato, "Hypoactivation of the prefrontal cortex during verbal fluency test in PTSD: a near-infrared spectroscopy study," Psychiatry Research: Neuroimaging, vol. 124, no. 1, pp. 1-10, Sep. 2003 [Online]. Available: View
- L. D. Morries, P. Cassano, and T. A. Henderson, "Treatments for traumatic brain injury with emphasis on transcranial near-infrared laser phototherapy," Neuropsychiatr Dis Treat, vol. 11, pp. 2159-2175, Aug. 2015 [Online]. Available: View
- L. M. Williams, A. H. Kemp, K. Felmingham, M. Barton, G. Olivieri, A. Peduto, E. Gordon, and R. A. Bryant, "Trauma modulates amygdala and medial prefrontal responses to consciously attended fear," NeuroImage, vol. 29, no. 2, pp. 347-357, Jan. 2006 [Online]. Available: View
- L. Sippel, "How does virtual-reality therapy for PTSD work?," Scientific American Mind, vol. 24, no. 5, pp. 74-74, 2013 [Online]. Available: View
- L. Zhang, W. Li, N. Shu, H. Zheng, Z. Zhang, Y. Zhang, Z. He, C. Hou, Z. Li, J. Liu, L. Wang, L. Duan, T. Jiang, and L. Li, "Increased white matter integrity of posterior cingulate gyrus in the evolution of post-traumatic stress disorder," Acta Neuropsychiatrica, vol. 24, no. 1, pp. 34-42, Feb. 2012 [Online]. Available: View
- M. A. Naeser, R. Zafonte, M. H. Krengel, P. I. Martin, J. Frazier, M. R. Hamblin, J. A. Knight, W. P. Meehan, and E. H. Baker, "Significant improvements in cognitive performance post-transcranial, red/near-infrared light-emitting diode treatments in chronic, mild traumatic brain injury: open-protocol study," J. Neurotrauma, vol. 31, no. 11, pp. 1008-1017, Jun. 2014.
- M. L. Cohen, R. H. Rozensky, Z. Z. Zlatar, R. N. Averbuch, and J. E. Cibula, "Posttraumatic stress disorder caused by the misattribution of seizure-related experiential responses," Epilepsy Behav, vol. 19, no. 4, pp. 652-655, Dec. 2010 [Online]. Available: View
- N. Kar, "Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: a review," Neuropsychiatric Disease and Treatment, vol. 7, pp. 167-181, 2011 [Online]. Available: View
- N. Mitsuhashi, K. Fujieda, S. Kawamoto, K. Okubo, T. Takagi, and T. Tamura, "BodyParts3D: 3D structure database for anatomical concepts," Nucleic acids research, vol. 37, no. Database issue, pp. D782-5, 2009.
- P. R. Porto, L. Oliveira, J. Mari, E. Volchan, I. Figueira, and P. Ventura, "Does cognitive behavioral therapy change the brain? A systematic review of neuroimaging in anxiety disorders," The Journal of Neuropsychiatry and Clinical Neurosciences, vol. 21, no. 2, pp. 114-25, 2009 [Online]. Available: View
- P. Stone, "Neuroimaging Study Claims To Distinguish TBI From PTSD." [Online]. Available: View
- Q. Wu, W. Xuan, T. Ando, T. Xu, L. Huang, Y.-Y. Huang, T. Dai, S. Dhital, S. K. Sharma, M. J. Whalen, and M. R. Hamblin, "Low-level laser therapy for closed-head traumatic brain injury in mice: effect of different wavelengths," Lasers Surg Med, vol. 44, no. 3, pp. 218-226, Mar. 2012.
- R. A. Lanius, R. L. Bluhm, and P. A. Frewen, "How understanding the neurobiology of complex post-traumatic stress disorder can inform clinical practice: a social cognitive and affective neuroscience approach," Acta Psychiatr Scand, vol. 124, no. 5, pp. 331-348, Nov. 2011.
- R. E. Propper and S. D. Christman, "Interhemispheric Interaction and Saccadic Horizontal Eye Movements: Implications for Episodic Memory, EMDR, and PTSD," Journal of EMDR Practice and Research, vol. 2, no. 4, pp. 269-281, 2008 [Online]. Available: View
- R. Patel, R. N. Spreng, L. M. Shin, and T. A. Girard, ">Neurocircuitry models of posttraumatic stress disorder and beyond: A meta-analysis of functional neuroimaging studies," Neuroscience & Biobehavioral Reviews, vol. 36, no. 9, pp. 2130-2142, Oct. 2012 [Online]. Available: View
- R. W. Gunter and G. E. Bodner, " EMDR Works . . . But How? Recent Progress in the Search for Treatment Mechanisms," Journal of EMDR Practice and Research, vol. 3, no. 3, pp. 161-169, 2009 [Online]. Available: View
- S. D. McDonald and P. S. Calhoun, "The diagnostic accuracy of the PTSD Checklist: A critical review," Clinical Psychology Review, vol. 30, no. 8, pp. 976-987, Dec. 2010 [Online]. Available: View
- S. F. Taylor and I. Liberzon, "Neural correlates of emotion regulation in psychopathology," Trends in Cognitive Sciences, vol. 11, no. 10, pp. 413-418, Oct. 2007 [Online]. Available: View
- S. Rossi, M. Hallett, P. M. Rossini, and A. Pascual-Leone, "Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research," Clin Neurophysiol, vol. 120, no. 12, pp. 2008-2039, Dec. 2009 [Online]. Available: View
- S. van Liempt, " Sleep disturbances and PTSD: a perpetual circle?," Eur J Psychotraumatol, vol. 3, Oct. 2012 [Online]. Available: View
- Steenkamp MM, Litz BT, Hoge CW, and Marmar CR, " Psychotherapy for military-related ptsd: A review of randomized clinical trials," JAMA, vol. 314, no. 5, pp. 489-500, Aug. 2015 [Online]. Available: View
- T. A. Henderson and L. Morries, "Near-infrared photonic energy penetration: can infrared phototherapy effectively reach the human brain?," Neuropsychiatric Disease and Treatment, p. 2191, Aug. 2015 [Online]. Available: View
- T. Harrington and E. Newman, "The psychometric utility of two self-report measures of PTSD among women substance users," Addictive Behaviors, vol. 32, no. 12, pp. 2788-2798, Dec. 2007 [Online]. Available: View
- T. Nagaoka, E. Kunieda, K. Sakurai, M. Taki, S. Watanabe, S. Watanabe, and Y. Yamanaka, "Development of realistic high-resolution whole-body voxel models of Japanese adult males and females of average height and weight, and application of models to radio-frequency electromagnetic-field dosimetry," Physics in medicine and biology, vol. 49, no. 1, pp. 1-15, 2004.
- T. W. Freeman, D. Cardwell, C. N. Karson, and R. A. Komoroski, "In vivo proton magnetic resonance spectroscopy of the medial temporal lobes of subjects with combat-related posttraumatic stress disorder," Magn. Reson. Med., vol. 40, no. 1, pp. 66-71, Jul. 1998 [Online]. Available: View
- W. Xuan, T. Agrawal, L. Huang, G. K. Gupta, and M. R. Hamblin, "Low-level laser therapy for traumatic brain injury in mice increases brain derived neurotrophic factor (BDNF) and synaptogenesis," J Biophotonics, vol. 8, no. 6, pp. 502-511, Jun. 2015.
- "In military and veteran populations, trials of the first-line trauma-focused interventions CPT and prolonged exposure" .
- "3_PTSD_CheckList_and_Scoring.pdf." [Online]. Available: View
- "7 Myths (and 1 Big Fact) about PTSD." [Online]. Available: View
- "Brain: Atlas of human anatomy with MRI," IMAIOS. [Online]. Available: View
- "Brodmann area," Wikipedia, the free encyclopedia. 13-Oct-2015 [Online]. Available: View
- "Definition - Temporal Lobe | Serendip Studio." [Online]. Available: View
- "Does Post-Traumatic Stress Disorder Require Trauma?" [Online]. Available: View
- "Headed for Trouble," Tufts Now. [Online]. Available: View
- "Mayo PTSD." [Online]. Available: View
- "Mild traumatic brain injury and posttraumatic stress disorder in returning veterans: Perspectives from cognitive neuroscience." [Online]. Available: View
- "My PTSD Forum," My PTSD Forum. [Online]. Available: View
- "New Study Discovers Near-Infrared Light Therapy (NILT) Effectively Treats Traumatic Brain Injury (TBI) Patients." [Online]. Available: View
- "PTSD - Scientific American," Scientific American - PTSD. [Online]. Available: View
- "PTSD Checklist for DSM-5 (PCL-5) - PTSD: National Center for PTSD." [Online]. Available: View
- "PTSD Screening Instruments - PTSD: National Center for PTSD." [Online]. Available: View
- "PTSDChecklistScoring PCL-17.pdf." [Online]. Available: View
- "PTSDChecklistScoring.pdf." [Online]. Available: View
- " Post Traumatic Stress Disorder and Addiction," Dual Diagnosis. [Online]. Available: View
- "Post-Traumatic Stress Disorder (PTSD)." [Online]. Available: View
- "Quantitative meta-analysis of neural activity in posttraumatic stress disorder." [Online]. Available: View
- "Shocking PTSD, suicide rates for vets," Face the Facts USA. [Online]. Available: View
- "Sleep disorders in combat-related PTSD." [Online]. Available: View
- "Sleep disturbance as the hallmark of posttraumatic stress disorder," AJP, vol. 146, no. 6, pp. 697-707, Jun. 1989 [Online]. Available: View
- "Snapshot." [Online]. Available: View
- "Snapshot." [Online]. Available: View
- "Snapshot." [Online]. Available: View
- "Snapshot." [Online]. Available: View
- "Snapshot." [Online]. Available: View
- "Snapshot." [Online]. Available: View
- "Snapshot." [Online]. Available: View
- "Soldiers' Stress: What Doctors Get Wrong about PTSD." [Online]. Available: View
- "Suicide and PTSD - PTSD: National Center for PTSD." [Online]. Available: View
- "Tetris Shown to Lessen PTSD and Flashbacks." [Online]. Available: View
- "The PTSD Solution: New Hope through Brain Plasticity," Psychology Today. [Online]. Available: View
- "These findings suggest that alterations of white matter integrity in PCG link to mnemonic and affective processing in PT." .
- "Traumatic Brain Injury Resource Guide - Temporal Lobes." [Online]. Available: View
- "Unemployment Biggest Predictor of PTSD Symptom Severity," Medscape. [Online]. Available: View
- "Who Benefits Most from PTSD Treatment?" [Online]. Available: View